We recently chatted with Forró about his work at the Chicago Biohub and the future of non-invasive biomedical research.
What kinds of research does your group conduct at the Chicago Biohub?
I’ve been particularly interested in the potential of patient-derived stem cell technology, which allows us to reprogram adult cells, like skin or blood cells, into stem cells and then grow virtually any human tissue — such as heart, lung or brain cells — in the lab. This approach lets us recreate disease-specific tissue in Petri dishes and then conduct detailed, real-time studies without needing to perform surgery on humans or work with animal proxies.
Where we come in is figuring out how to study the tissue that’s grown with some sort of disease, such as epilepsy or Parkinson’s. You need to measure the electrical activity, the chemical contents, neurotransmitters, and all their inter-related dynamics. So my group builds instruments that collect data from those tissues. But these devices don’t just record data — we can also stimulate cells or test potential medical interventions directly in human tissue samples. For example, right now we’re building devices for stretching lab-grown skin to help study psoriasis, which is a disease that seems to get exacerbated in regions where the skin stretches a lot.
In what ways do you hope to advance the field of biomedical research?
My postdoctoral research at Stanford was mainly focused on developing devices that could sense electrical signals from neural tissue samples. Now, my group at the Biohub is expanding on that vision significantly. We’re creating platforms that can also deliver drugs, collect fluids, and detect key biomolecules like dopamine, cytokines, and other signaling compounds critical to tissue function.
What excites me most is the idea of creating closed-loop systems, which are devices that not only sense and respond to cellular environments, but also learn over time. We’re incorporating artificial intelligence into our devices so they can interpret patterns and adjust their behavior to promote healing or suppress disease states. In the long term, I see our work contributing to smart therapeutic platforms that offer real-time intervention strategies tailored to the individual biology of a patient.
Wow, so you’re planning on giving these devices the ability to learn. How might these smart devices someday be used to treat disease?
Imagine a patient with a genetic form of epilepsy. Using skin cells from that individual, we can grow miniature brain-like structures, called brain organoids, in the lab. My team is building devices that can be embedded inside these organoids and both monitor and stimulate the tissue.
Over several months, a machine learning algorithm could monitor electrical activity, learn to recognize early seizure signatures, and test different methods of intervention — whether electrical or chemical. This approach allows us to explore patient-specific therapies in a lab setting well before moving to clinical trials. It’s a powerful new way to investigate treatment strategies tailored to individual biology.
There are a lot of challenges to designing devices that can interface with biological samples. If a sensor contains toxic materials, or the structure is too rigid, it can damage living tissue. The shape, temperature, and moisture of tissue samples can also destroy sensors. What are some of the innovative techniques your group is working on to design devices that integrate seamlessly with living tissue?
While engineers have used software to design devices for decades, much of that work still relies on manually sketching structures with rigid geometries like squares, rectangles, and straight lines. But biological tissues are soft, curved, and dynamic. They don’t respond well to having conventional, blocky hardware shoved into them. In my group, we’re developing computationally driven design workflows that are specifically tailored to organic structures.
As these devices get more complex, you need automated computational methods to optimize their designs to fit biological forms. We integrate these optimization algorithms to answer critical questions from the outset: Can this device survive 300 days in a humid incubator at 98 degrees? Will it hold up under vibrations or the weight of growing tissue? You need designs that are robust, flexible, and tissue-compatible — and for that, computational design and the capacity to quickly iterate are essential. It enables us to move quickly, refine our prototypes, and test biologically realistic conditions before fabrication.
What building approaches do you take when turning these digital designs into physical devices?
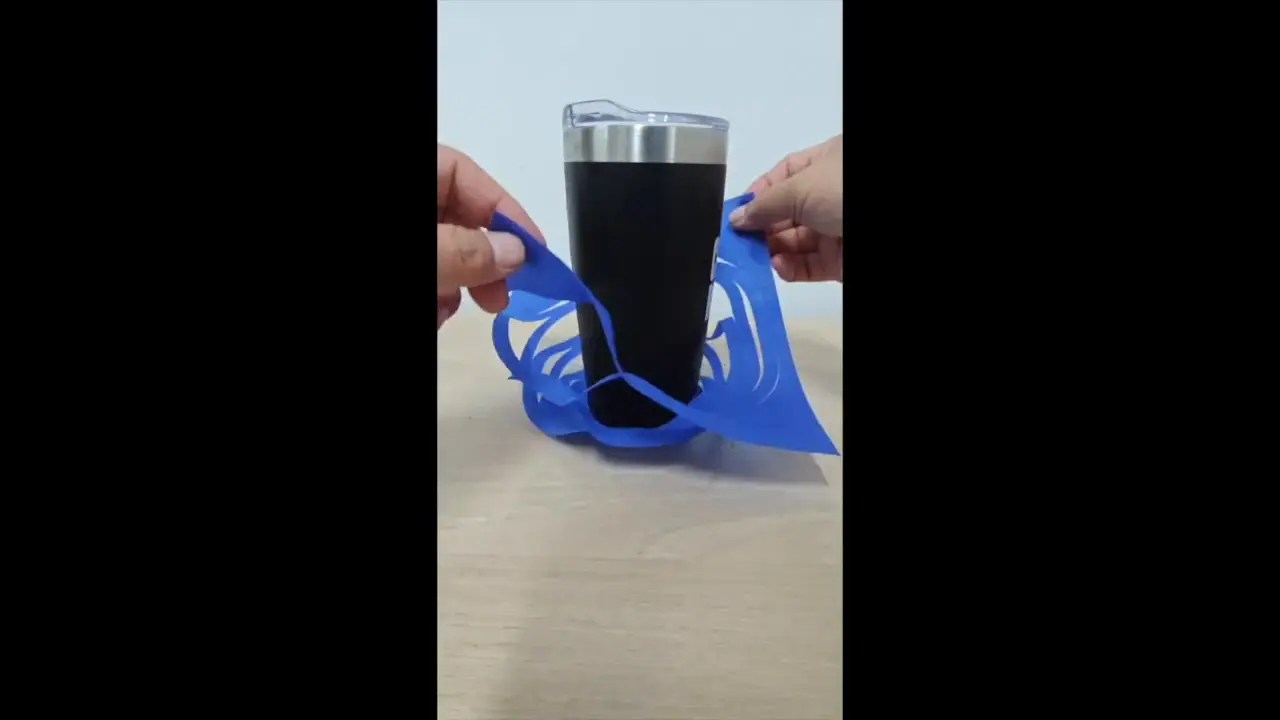
Traditional approaches to studying lab-grown tissues often rely on invasive techniques, such as inserting electrodes or sensors directly into delicate samples. But this can cause significant physical damage, making it difficult to distinguish between the actual effects of a disease and the consequences of the instrumentation itself. In my lab, we’ve developed an alternative approach: building ultra-thin, flexible devices that are effectively “consumed” by the tissue as it grows. Instead of forcing hardware into the sample, we allow the tissue to naturally envelop the device over time, forming a seamless interface.