Pete Farley
Director of Communications
Comprehensive mapping of pathogen populations points way to precision treatments to improve outcomes
May 28, 2024

For children who undergo bone marrow transplants, even mild respiratory infections can turn deadly. Now, using a sophisticated method that rapidly and comprehensively identifies all potentially pathogenic organisms present in the lungs, an international research team including scientists at UC San Francisco (UCSF) and Chan Zuckerberg Biohub San Francisco (CZ Biohub SF) have discovered links between certain microbial communities and the relative risk of mortality in these patients.
The new study, published May 23, 2024 in Nature Medicine, points the way to more precise diagnostics, and eventually therapeutics, to improve children’s survival rates after transplant.
The research team, which included dozens of researchers from hospitals in the U.S., Canada, and Australia, enrolled a broad cohort of pediatric patients and used a technique called metagenomic next-generation sequencing (mNGS) to analyze fluid collected from the lungs.
After determining the relative abundance of the various microbes present in each of these samples, the researchers categorized patients in four distinct “clusters” that allowed them to predict which children were most susceptible to fatal lung injury. They found that, compared to other clusters, children with the worst outcomes had significantly fewer microbial species overall, but marked populations of Staphylococcus bacteria and viruses.
“We took samples from 229 pediatric bone marrow transplant patients across 32 hospitals,” said first author Matt Zinter, assistant professor of pediatrics at UCSF. “Our results, which we validated in an entirely separate cohort, indicate that lung microenvironments are predictive, or prognostic, for the risk of mortality. Our ultimate goal is to figure out how to modulate pulmonary biology for the benefit of our patients.”
Bone marrow transplant, also known as hematopoietic cell transplantation (HCT), is a life-saving treatment for children battling leukemia, bone marrow failure, and genetic disorders such as inborn immunodeficiencies and sickle-cell disease, but the procedure is grueling. It involves administering high doses of chemotherapy to kill off diseased cells in the bone marrow, which suppresses the immune system but facilitates the growth of healthy stem cells that are later transplanted into patients.
This immune suppression renders patients exceptionally vulnerable to viruses, bacteria, and other pathogens that enter the body during the critical phase of immune system “rebooting.”
“We see these patients in the ICU, and they’re among the sickest patients that are seen in a children’s hospital,” said Zinter, a pediatric critical care specialist and program director for Pediatric Immunocompromised Critical Care at UCSF Benioff Children’s Hospitals. Zinter conducts research in the laboratory of CZ Biohub SF President Joseph DeRisi, professor of biochemistry and biophysics at UCSF.
Lung infections are particularly common in this group, affecting as many as 40% of pediatric HCT patients. When children with infection-related lung injuries need to be placed on ventilators, mortality rates approach 50%.
“But with hundreds of potential types of pathogens invading the lungs, how do doctors who order traditional tests know they’re testing for the right ones?” said DeRisi, senior author of the study. “The metagenomic sequencing technology we’ve used in this study is unbiased and hypothesis-free — you’re not guessing what organisms are present in a sample.”
As an alternative to traditional diagnostic methods that target specific organisms, such as culturing, DeRisi, Zinter, and colleagues in the Pediatric Transplantation and Cell Therapy Consortium turned to mNGS. The researchers first obtained fluid from the lungs of study participants and sequenced the total RNA in each sample to detect every type of microorganism present, without regard to whether they are known to be pathogenic.
When the researchers uploaded this sequencing data to Chan Zuckerberg ID, a free, cloud-based metagenomic platform, they were surprised to discover that several microorganisms other than bacteria and viruses were present, including Toxoplasma gondii, a parasite found in cat feces; Acanthamoeba, an amoeba found in soil; and the fungi Cryptococcus and Pneumocystis.
“Pulmonary infections in HCT patients are complex — there might be common microbes causing them, but also very rare and uncommon microbes,” said Zinter. “We’ve found organisms that physicians treating these patients likely aren’t even aware of because there is not currently a good clinical test available for them.”
Based on the microbiome composition of the patients’ lungs, the researchers classified participants into four clusters, and determined the clinical outcomes for each group. Patients in the cluster associated with the highest mortality, whose lungs exhibited inflammation and cellular damage, showed a significant overall depletion of microbial species in their lung microbiome, but there were conspicuous populations of Staphylococcus and viruses.
“There’s a delicate balance between the microbiome blossoming so big that it represents infection, or contracting to the point that it’s depleted and non-existent,” said Zinter. “It’s like the Goldilocks analogy — the middle ground seems to be just right.”
In short, Zinter said, the more abnormal the immune environment in the lungs, the more abnormal the lung microbiomes uncovered in the study, and the higher the rate of infections.
The researchers also found a strong link between antibiotic treatment and bacterial depletion, accompanied by enriched communities of viruses and fungi. Because sicker patients tend to receive more antibiotics, disentangling microbial causes of mortality is not straightforward, they said.
“Metagenomics is a realistic way forward to improve outcomes for children after HCT,” said DeRisi, “It offers a wealth of real-time information about what’s going on in these patients, so their doctors can make life-saving decisions.”
###
About the Chan Zuckerberg Biohub San Francisco
CZ Biohub San Francisco, part of the Chan Zuckerberg Biohub Network, is a nonprofit biomedical research center founded in 2016. CZ Biohub SF’s researchers, engineers, and data scientists, in collaboration with colleagues at our partner universities — Stanford University; the University of California, Berkeley; and the University of California, San Francisco — seek to understand the fundamental mechanisms underlying disease and develop new technologies that will lead to actionable diagnostics and effective therapies. Learn more at czbiohub.org/sf.
About UCSF
The University of California, San Francisco (UCSF) is exclusively focused on the health sciences and is dedicated to promoting health worldwide through advanced biomedical research, graduate-level education in the life sciences and health professions, and excellence in patient care. It includes UCSF Health, which comprises three top-ranked hospitals, as well as affiliations throughout the Bay Area. Learn more at https://www.ucsf.edu, or see our Fact Sheet.
Stay up-to-date on the latest news, publications, competitions, and stories from CZ Biohub.
Marketing cookies are required to access this form.
 News Releases
News Releases
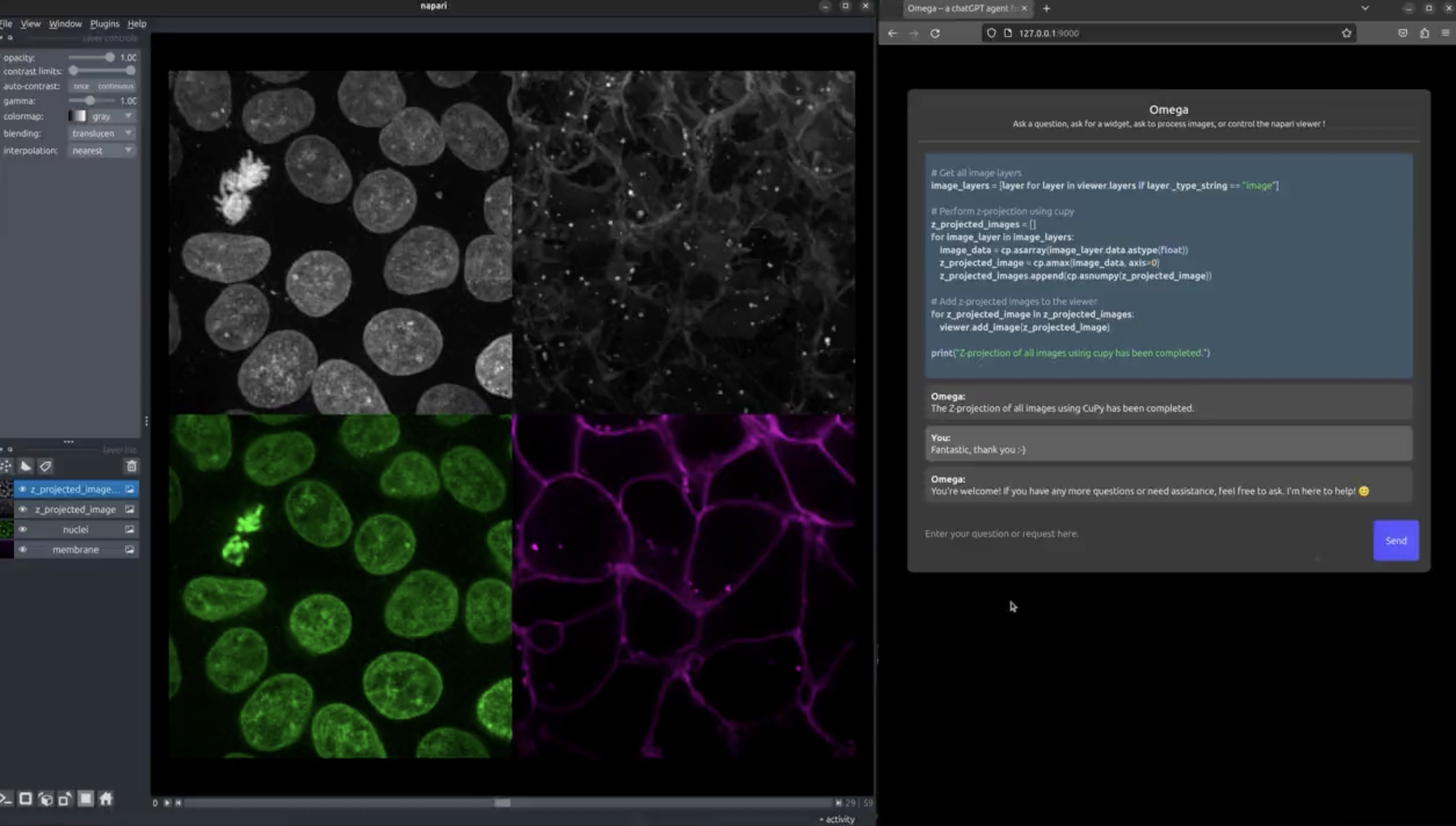
By lowering technical barriers, Omega democratizes image analysis ...
 News Releases
News Releases
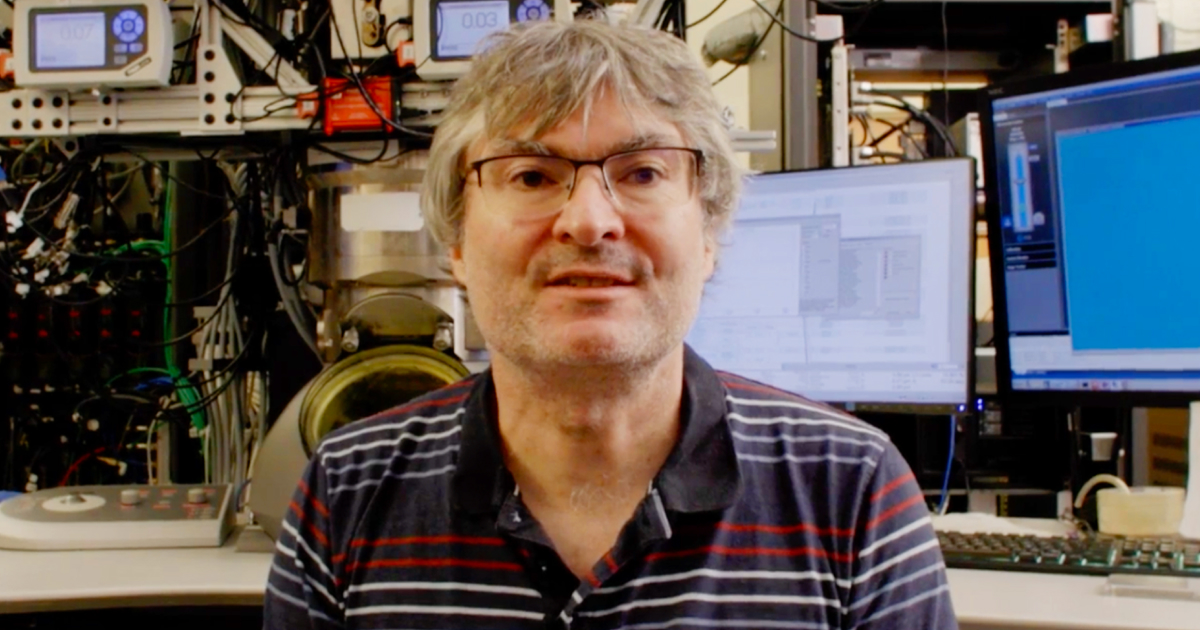
Join scientist Holger Müller in his lab, which is developing innovative imaging technology that may hold the key to unlocking new insights into our ...
 News Releases
News Releases
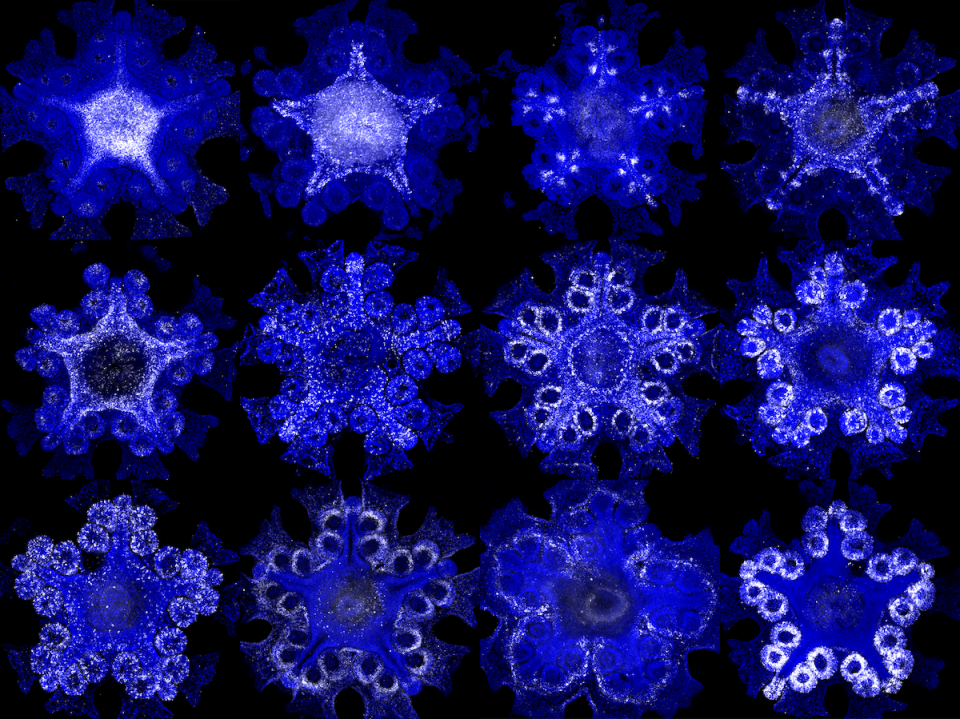
Collaboration led by CZ Biohub SF Investigators unveils a new understanding of the sea star body plan ...
Stay up-to-date on the latest news, publications, competitions, and stories from CZ Biohub.
Marketing cookies are required to access this form.